- When does Urinary Incontinence occur?
- What is the impact of Incontinence on Quality of Life?
- How is Urinary Incontinence diagnosed?
- What are the types of Urinary Incontinence?
- Stress Incontinence (Effort Incontinence)
- What is the etiology of Stress Incontinence?
- Treatment of Stress Incontinence
- Urge Incontinence
- Treatment of Urge Incontinence
- What is Mixed Incontinence?
- Overflow Incontinence
Urinary Incontinence is a general term used to describe any involuntary loss of urine. It is not a disease; it is a symptom.
When does Urinary Incontinence occur?
Women are three times more likely to present incontinence compared to men. The probaility of developing incontinence increases with age, without though being considered a natural consequence of aging. It is estimated that at least 1 out of 10 women 40-65 years old and 3 out of 10 women over 65 years old face this problem.
What is the impact of Incontinence on Quality of Life?
Urinary incontinence is accompanied with feelings of embarrasment, low self-confidence and reduced sexual and social activity. Very often the woman or man with incontinence ends up using diapers; as a result, besides the hygiene issues and health problems induced, patients are led to social isolation. In many cases, incontinence results in depression, with dramatic impact on the quality of life of both patients and their close people.
Even though at least 7 out of 10 incontinence cases could be treated successfully, unfortunately more than half of those suffering do not seek medical help; instead they just resort to non-medical sources of information and usage of diapers!
How is Urinary Incontinence diagnosed?
The diagnosis of the problem is based on the patient's detailed medical history. The physician collects important information about the type of disturbances, the character of incontinence, severity degree, time and frequency of occurrence. You may be asked to fill in special questionnaires, and even keep a urine diary for recording how many times you urinate, what time of the day or night and how many liquids you consume -for 3 consecutive days. Then follows the clinical examination -including gynecological examination for women and digital prostate examination for men- and neurological evaluation. You may also be asked to have general urine tests, urine culture, and probably some blood tests.
Monitoring is completed with UltraSound screening tests of the kidneys, bladder and genitalia. In some cases, Cystoscopy may be also performed (endoscopic examination of the bladder through the urethra, with the use of a special tube having a small camera, a cystoscope, on its end). Lastly, in special cases, there is need for radiological screening, such as Cystourethrography, and CT-scan.
What is Urodynamic Testing?
It is the most specialized test for urinary incontinence. It aims at investigating the bladder and urethral function with accuracy, by stimulating the process of filling and voiding of the bladder. It is conducted with the use of a special device and by inserting a catheter into the bladder to measure stress within the bladder and urethra. However, the most widely used test is Uroflowmetry: the patient urinates into a special device measuring the flow and amount of urine released. After the test, it is important to measure -with the use of ultrasounds- whether there is post-void urine residual (PVR) in the bladder. Should there be over 100ml post-void residual urine, the condition is considered to be pathological and may cause urinary tract infections. Contemporary studies have shown that with this residual urine the bladder is not able to complete its normal function, that is voiding.
It should be emphasized that the aim of all these tests is to help the physician identify the type of urinary incontinence and its etiology, so as to decide on the proper therapeutic strategy.
What are they types of Urinary Incontinence?
There are 3 types of incontinence differing from each other with regard to their etiological mechanism, manifestation and treatment:
- Stress Incontinence (Effort Incontinence)
- Urge Incontinence
- Overflow Incontinence
Stress Incontinence (Effort Incontinence)
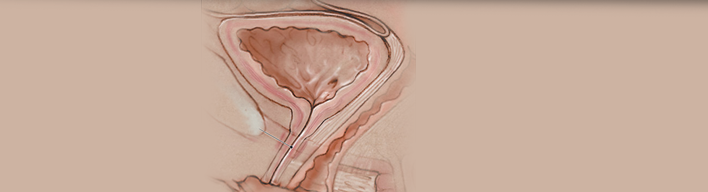
Involuntary loss of urine when performing some effort (for example with body movements, when exercising, coughing or sneezing). When intraabdominal stress increases, there is higher pressure exerted on the urethral sphincter (muscle preventing the exit of urine from our bladder). This mechanism normally remains closed as the bladder fills with urine; in the case of incontinence, however, it is insufficient during effort. As a consequence, the pressure exerted is higher than the sphincter's resistance and there is leakage of urine.
Daily activities that increase intraabdominal pressure are:
- when making an effort to get up from bed or from a low seat
- when making an effort to lift weights, e.g. carrying bags with daily groceries or a small child
- when walking up stairs
- when exercising, dancing or even during sexual activity
- when laughing or coughing
What are the causes of Stress (Effort) Incontinence?
The most common etiology involves changes in the urinary tract anatomy, or in the pelvic floor (muscles supporting organs within the pelvis) or impairment of the nerves controlling these muscles. Another potential cause may be dysfunction or injury of the urethral sphincter.
The role of gestation in incontinence
The above mentioned changes may occur due to gestation,as the fetus grows up within the pelvis and presses abdominal and pelvic organs. During delivery, the pelvic floor muscles stretch together with the vagina and may become loose. As a consequence, the position of the urethra changes, while in some cases it may even result in Pelvic Organ Prolapse (POP). When there is bladder prolapse, the condition is called Cystocele. When there is Rectal Prolapse, the condition is called Rectocele. When both conditions co-exist, we have Cystorectocele.
That is why, women should follow a special exercise program -both during gestation and immediately after gestation- for restoring pelvic floor muscles and, thus, preventing incontinence.
Menopause
During menopause many hormonal changes take place: vaginal secretions are reduced, the vagina dries out and gradually loses its elasticity due to oestrogen deficiency and also affects the overlying urethra. Lastly, obesity, smoking and chronic cough favour the occurrence or aggravation of incontinence.
When there is sphincter impairment
Incontinence may also occur due to impairment of the sphincter or sphincter nerves, that may be observed after pelvic organ surgery (e.g. hysterectomy in women and prostatectomy in men) or after surgery for bladder, prostate and intestinal cancer.
Neurogenic Bladder
Neurological diseases or injuries may also cause urinary incontinece due to impairment of the bladder and sphincter nerves. Such case are multiple sclerosis (MS), spinal cord and spinal injuries, parkinsonian disorders, strokes etc.
Treatment of Stress (Effort) Incontinence
Treatment for Stress Incontinence depends on the severity of the problem and its etiology, but also on the patient's expectations. There are more and less invasive techniques and very often there is combination of therapies.
Physiotherapy and Pelvic Floor Exercises
Physiotherapy, combined with Bio-feedback, aims at strengthening pelvic floor muscles (muscles supporting the urethra and bladder). In mild and moderate incontinence cases, physiotherapy can resolve the problem. It is recommended that physiotherapy takes place with the assistance of a specialised Physiotherapist. It can also be used in combination with pharamaceutical agents facilitating sphincteric contraction.
Tension-Free Tape Surgery
In cases of severe stress incontinence and when conservative treatment fails, we move on to surgical treatment. Today, the treatment of choice is considered to be the 'Tension-Free Vaginal Tape' (TVT). A tape is placed below the urethra to provide support for the area where the bladder meets the urethra. The tape may be made of natural or artificial material. In 80-90% of cases, stress incontinence is cured following this technique. Potential side effects include recurrence and changes in micturition.
During the last years, the tension-free tape under the urethra has been applied to resolve also male stress incontinence, particularly following prostatectomy.
In case there is also bladder or rectal prolapse, special meshes are placed within the vagina, in the same way as happens with tension-free tapes.
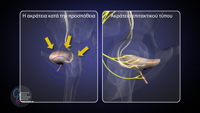
The Artificial Sphincter
In cases of severe sphincter impairment, the only effective solution is the placement of an artificial sphincter. This is a mechanism that is surgically placed around the sphincter and connected with a water pump. The artificial sphincter is usually used in males with incontinence after prostatectomy.
Urge Incontinence
What is Urge Incontinence and Overactive Bladder?
The urgent feeling to urinate normally arises only when the bladder is completely full and we are normally able to control bladder contraction -something that we do every time we urinate. In Urge Incontinence, the patient often has an urgent feeling for micturiotion which cannot be postponed despite the fact that the bladder is not full. It is usually accompanied with urine leakage.Patients may mistake high urinary frequency for urinary tract infection; however, here there is absence of the other urinary tract infection symptoms, such as pain and hematuria.
What are the causes of Overactive Bladder?
In most cases the Overactive Bladder Syndrome is of unclear etiology related to hypersensitivity of bladder nerves. In some cases, however, it may be associated with some neurological disease (e.g. multiple sclerosis, spine injuries, stroke); in these cases, it is called 'Neurogenic Bladder'. In men, the most common cause is chronic obstruction and inability of urine to exit, as happens in prostate hypertrophy or urethral stricture. Very often, it is accompanied with nocturia (urinating in the night).
Treatment of Urge Incontinence
Urge Incontinence is treated pharmaceutically. Today there are special medications inhibiting involuntary bladder contractions. These are called anticholinergic agents (anticholinergics).
How do Anticholinergics act?
Bladder fucntion is controlled by nerves terminating to its wall. These nerve endings secrete substances that induce either relaxation of the bladder -during its filling phase- or contraction of the bladder -during its voiding phase. Anticholinergic agents act on these specific nerve endings, called 'bladder receptors' and are administered to change bladder function. In other words, anticholinergics act on bladder nerve receptors and inhibit bladder involuntary contractions.
Are Anticholinergics safe and effective?
These drugs are highly effective and safe. Main side effects are xerostomia and constipation. However, modern pharmaceutical agents have fewer adverse events while being equally effective or even more effective than the older ones.
When oral drugs are not effective
- In refractory cases that do not respond to oral pharmacotherapy, there is the option of Botulinum Toxin injections (BTX) or Transcutaneous Electric Nerve Stimulation (TENS). Botulinum Toxin, mostly known with its commercial name 'Botox', has been widely used worldwide with great efficacy and good safety. In this case, the agent is injected to specific sites of the bladder through a special endoscope, the cystoscope, with the use of a fine needle. The drug blocks the function of the nerves that are responsible for involuntary bladder contractions. This treatment has to be repeated every 6-12 months.
- In Transcutaneous Electrical Nerve Stimulation (TENS), bladder function is modified with the use of electric current that is supplied to the spine through a battery that is implanted in the buttock. The treatment is effective in 7 out of 10 patients. The battery has to be replaced every 7 years.
What is Mixed Incontinence?
Effort Incontinence and Urge Incontinence often co-exist, that is urine leaks both when abdominal muscles contract and when there is urinary frequency and urge. This phenomenon is called mixed-type incontinence. In such a case, we should identify which of the two types of incontinence causes the greatest disturbance in order to treat it first.

Overflow Incontinence
Loss of urine occurring when the amount of urine within the bladder overexceeds the limit to which the bladder usually empties. Then the pressure forced by the urine is much higher than sphincter resistance and there is leakage of urine. Common causes are chronic inability to urinate in men with prostate hypertrophy, as well as neurological impairment resulting in inability of the bladder muscle to void the urine -as happens, for example, in patients with diabetes mellitus and bladder neuropathy.
Knowldedge and therapeutic methods related to urinary incontinence have advanced impressively during the last years and offer today both prevention practices and therapeutic rehabilitation potentials. The initial step for resolving the problem is to visit a Urologist or Uro-Gynecologist and get promptly and properly informed about it.